
The Edinburgh Postnatal Depression Scale (EPDS) is a widely used, validated screening tool designed to identify symptoms of postpartum depression and anxiety in new mothers. It helps healthcare providers recognize emotional distress early, improving outcomes for both mother and child through timely support and intervention.
Early Detection of Postpartum Depression
Screens for emotional and psychological distress that may otherwise go unnoticed in new mothers.
Validated and Reliable Tool
Backed by extensive research, the EPDS provides consistent and accurate results across diverse populations.
Streamlined Mental Health Referrals
Supports decisions for timely counseling, psychiatric evaluation, or behavioral health intervention.
Improved Maternal and Infant Outcomes
Helps reduce the impact of untreated postpartum depression on bonding, breastfeeding, and child development.
Supports Quality of Care Initiatives
Contributes to maternal mental health monitoring in value-based care and quality reporting programs.
OB/GYN PracticesRoutine postpartum checkups to assess emotional wellbeing at 6 weeks and beyond.
Family Medicine Clinics
Integrated screenings during newborn or well-woman visits.
Pediatric Offices
Maternal mental health checks during infant well-checks, as part of whole-family care.
Midwife and Birth Center Care
Used during postnatal visits to identify patients in need of support.
Public Health and Community Clinics
Screening in programs for underserved populations or home visit programs.
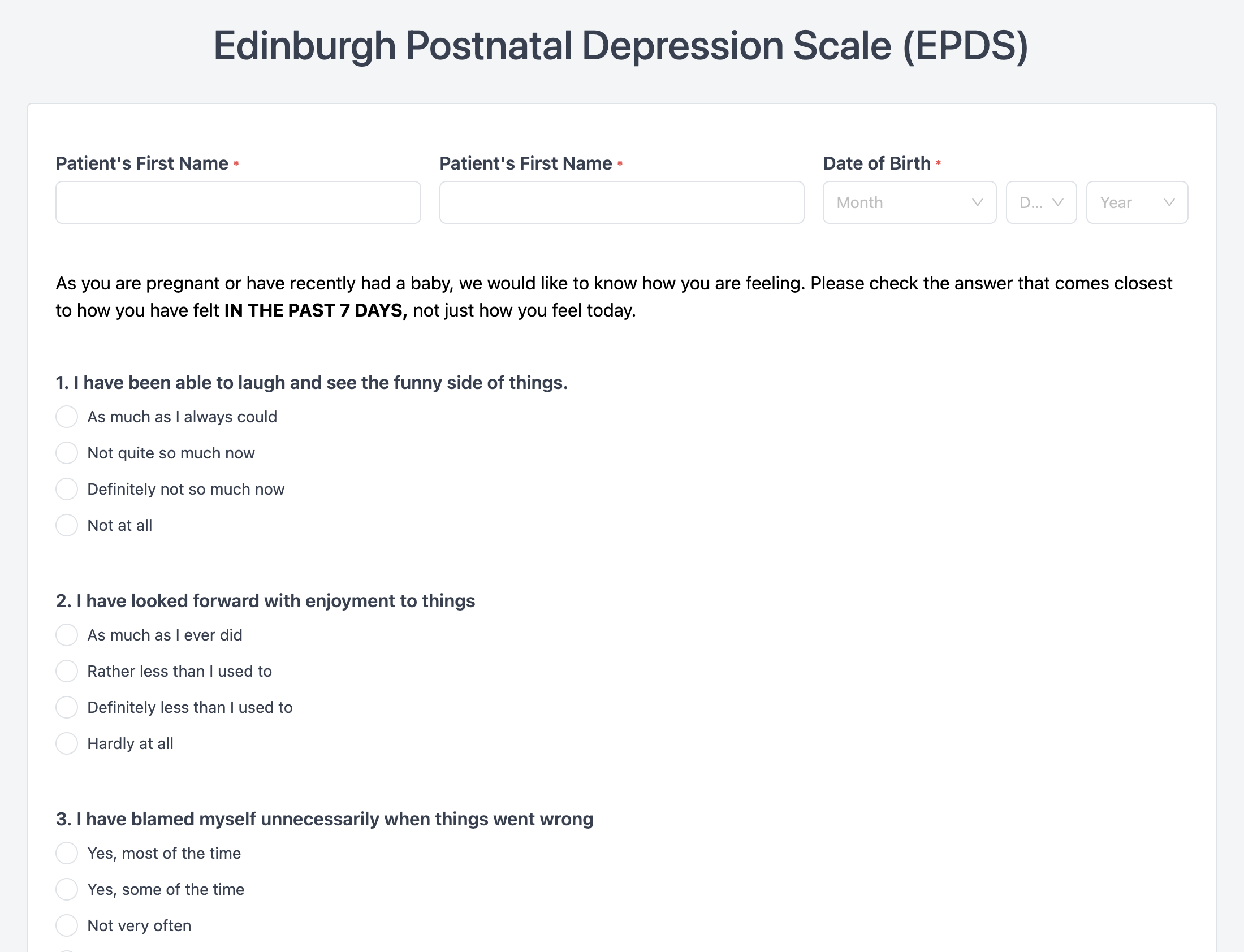
10 Questions:
Focus on mood, anxiety, guilt, sleep disturbance, and thoughts of self-harm—reflecting the mother’s emotional state over the past 7 days.
Scoring System:
Each item is scored 0–3, with a maximum possible score of 30.
Interpretation Guidelines:
Clinically Meaningful Change:
Reductions of 3+ points often signal significant improvement in mood or treatment response.
Standard Screening Point:
Administer at 6-week postpartum visit or earlier if risk factors are present.
Multiple Screening Opportunities:
Repeat at 3 and 6 months postpartum, or during infant checkups when appropriate.
Patient Instructions:
Ensure privacy and a quiet setting; stress the importance of honest responses based on the past 7 days.
Score Review Protocols:
Establish clear referral pathways for scores indicating moderate or severe distress.
EMR Integration:
Document EPDS scores and actions taken within clinical notes or mental health sections of the EMR.