
The Foot and Ankle Disability Index (FADI) is a validated, patient-reported outcome measure designed to assess functional limitations and disability related to foot and ankle conditions. This standardized assessment tool helps clinicians quantify patient symptoms, track treatment progress, and demonstrate outcomes for various foot and ankle disorders.
Objective Outcome Measurement: Quantify patient-reported disability levels with a reliable, validated scoring system that provides consistent measurement across patients and time.
Treatment Progress Tracking: Monitor patient improvement throughout treatment with standardized scores that clearly demonstrate functional gains or limitations.
Insurance Documentation: Provide objective evidence of functional impairment and treatment effectiveness required for insurance authorization and reimbursement.
Research and Quality Improvement: Collect standardized data for clinical research, practice quality improvement, and comparison with published treatment outcomes.
Patient Communication: Help patients understand their functional status and treatment progress through clear, numerical scoring systems.
Orthopedic Practices: Pre and post-surgical assessments for foot and ankle procedures, fracture recovery monitoring, and conservative treatment outcomes.
Physical Therapy Clinics: Initial evaluations, progress assessments, and discharge planning for patients with foot and ankle dysfunction.
Sports Medicine Centers: Athletic injury assessments, return-to-sport evaluations, and performance outcome tracking.
Podiatry Practices: Comprehensive foot disorder evaluations, treatment planning, and long-term outcome monitoring.
Workers' Compensation Evaluations: Functional capacity assessments for work-related foot and ankle injuries and disability determinations.
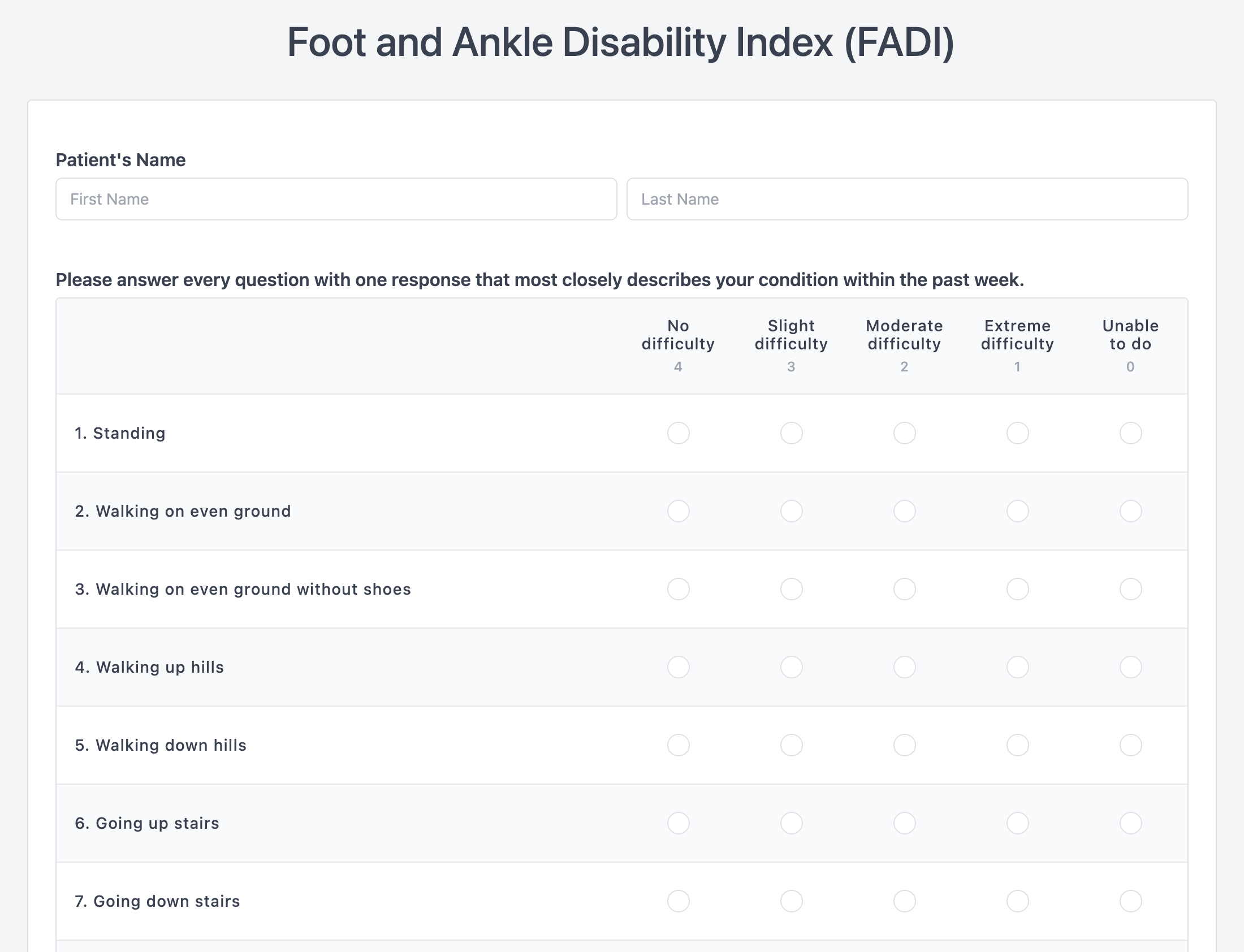
Activities of Daily Living Subscale (FADI-ADL): 21 items assessing basic functional activities including walking, stair climbing, and routine daily tasks.
Sports Subscale (FADI-Sport): 8 items evaluating higher-level activities including running, jumping, and sport-specific movements.
Scoring System: Each item scored 0-4 (no difficulty to unable to do), with total scores converted to percentages for easy interpretation.
Interpretation Guidelines: Higher scores indicate better function, with score changes of 8-12 points considered clinically meaningful improvements.
Initial Assessment: Administer at baseline to establish functional status before treatment begins.
Follow-up Scheduling: Re-administer at regular intervals (2-4 weeks) during active treatment and at discharge.
Patient Instructions: Provide clear instructions for completion, emphasizing answers should reflect current ability level.
Score Interpretation: Train staff to calculate and interpret scores consistently across all patients and providers.
Documentation Integration: Include FADI scores in treatment notes, progress reports, and discharge summaries.
Electronic Administration: Digital versions that patients can complete on tablets or computers in the clinic or at home.
Automated Scoring: Software that calculates scores automatically and flags significant changes for clinical review.
Progress Tracking: Visual displays of score changes over time to enhance patient motivation and clinical decision-making.
Quality Measures: Demonstrate treatment effectiveness for quality reporting requirements and accreditation standards.
Outcome Documentation: Provide objective evidence of functional improvement for insurance reviews and appeals.
Value-Based Care: Support participation in value-based payment models that reward improved patient outcomes.