
The Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire is a validated, self-reported tool used to assess physical function and symptoms in people with upper extremity disorders. It measures how arm, shoulder, or hand conditions affect daily activities, helping clinicians evaluate severity, monitor progress, and document treatment outcomes.
Standardized Functional Assessment
Provides consistent, quantifiable measurement of upper limb disorder across time and patient populations.
Track Recovery Over Time
Re-administer to observe changes in patient-reported symptoms and function during treatment.
Insurance Justification
Supports medical necessity and treatment effectiveness with objective, reproducible data.
Improved Patient Communication
Gives patients a clear understanding of their functional limitations and recovery trajectory.
Research and Quality Metrics
Enables data collection for studies, outcome reporting, and compliance with quality initiatives.
Orthopedic Clinics
Monitor recovery from fractures, tendon injuries, or surgeries involving the arm, shoulder, or hand.
Physical & Occupational Therapy
Establish functional baselines and track therapy progress for patients with upper extremity impairments.
Sports Medicine
Evaluate athletes recovering from shoulder dislocations, rotator cuff tears, or elbow injuries.
Rehabilitation Medicine
Assess disability in neurological or post-stroke patients with upper limb involvement.
Workers’ Compensation Evaluations
Determine work-related disability and return-to-work readiness for job-specific functional tasks.
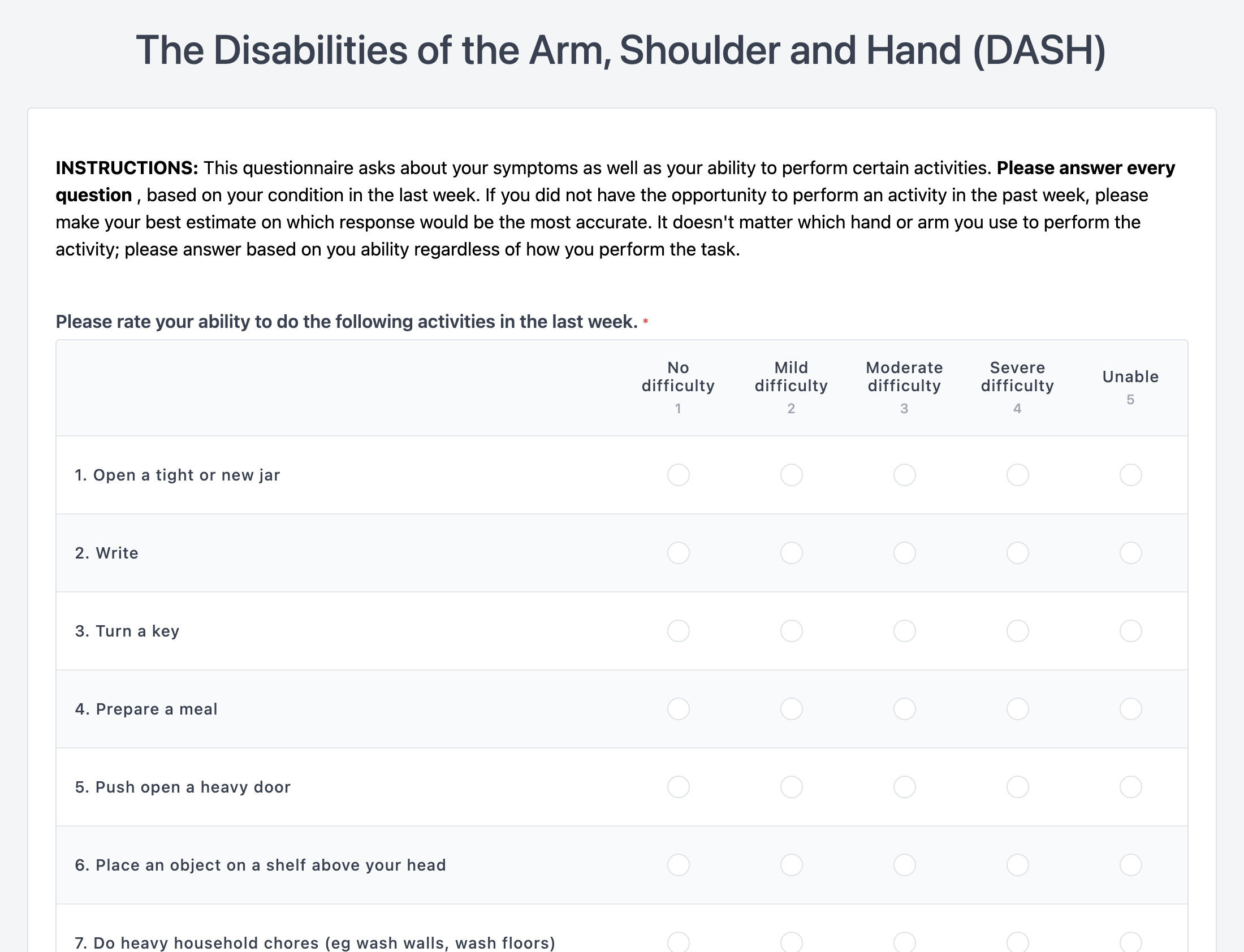
Core Questionnaire:
Optional Modules:
Scoring System:
Each item is scored 1–5. Total score is calculated as a percentage (0 = no disability, 100 = most severe disability).
Interpretation Guidelines:
Lower scores reflect better function. A change of 10 points or more is considered clinically significant.
Initial Assessment:
Administer at intake to establish a functional baseline.
Regular Follow-up:
Re-administer every few weeks or at discharge to track progress.
Patient Instructions:
Encourage honest, current-state responses reflecting the past week.
Score Review and Integration:
Train clinicians to interpret scores and include them in progress notes and care plans.